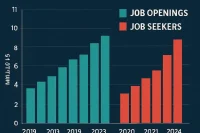
The American healthcare system is facing a healthcare staffing shortage in 2025 that no amount of technology or financial investment can easily solve: there simply aren’t enough doctors. A new nationwide survey of more than 1,000 physicians reveals a stark warning—63% of doctors believe there are not enough qualified physicians to fill current openings.
This shortage is not new, but it is intensifying. As patient demand grows with an aging population, burnout drives more doctors to leave the field, and medical school pipelines fail to keep up, the U.S. risks entering a prolonged healthcare staffing crisis. The consequences are severe: longer wait times, diminished access to care, and deepening health inequities.
The Numbers Behind the Shortage
- Projected Deficit: The Association of American Medical Colleges projects a shortfall of up to 124,000 physicians by 2034.
- Primary Care Gap: Nearly 40% of physicians say primary care is already in crisis, with rural and underserved communities hardest hit.
- Retirement Wave: Nearly one-third of current physicians are over the age of 60 and expected to retire within the next decade.
- Burnout Exit: Roughly 50% of practicing doctors report symptoms of burnout, and 1 in 5 have considered leaving the profession early.
The Worsening Healthcare Staffing Shortage in 2025: What You Need to Know
1. Aging Population, Rising Demand
The U.S. population over 65 is growing rapidly, creating higher demand for chronic disease management, preventive care, and specialized services. More patients require more doctors.
2. Medical Training Bottleneck
While applications to medical school have increased, the number of federally funded residency slots has barely grown in decades. Thousands of qualified graduates are left unmatched each year, unable to practice medicine despite years of training.
3. Physician Burnout
High administrative burdens, long hours, and pressure from electronic health record systems are driving burnout. Many physicians reduce their hours, retire early, or leave clinical practice altogether.
4. Consolidation and Cost Pressures
Mergers among hospital systems and insurance-driven cost controls add to stress, limiting physician autonomy and discouraging new entrants.
Impact on Patients
The physician shortage is already reshaping how patients experience healthcare:
- Longer Wait Times: Appointments with primary care doctors can now take weeks to secure.
- Specialty Delays: Access to dermatologists, neurologists, and psychiatrists can require months of waiting.
- Geographic Disparities: Rural communities are disproportionately affected, with many counties having no practicing specialists.
- Quality of Care: Overburdened physicians with too many patients risk shorter visits and rushed decisions.
Struggling to Hire Healthcare Professionals?
Post your openings on WhatJobs and connect with qualified doctors, nurses, and specialists fast.
Post a Job Now →Industry Response
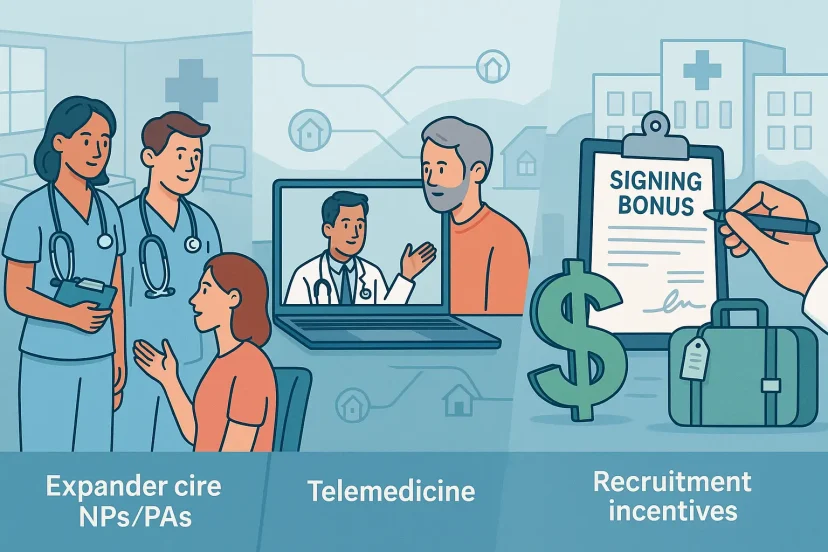
Expanding Roles for Non-Physician Providers
Nurse practitioners (NPs) and physician assistants (PAs) are filling some of the gaps, particularly in primary care. Their ranks have grown rapidly, with many states expanding their scope of practice.
Telemedicine Growth
Virtual care helps extend physician reach, especially in rural areas. However, it cannot replace hands-on specialties or emergency medicine.
Recruitment Incentives
Hospitals and clinics are offering signing bonuses, loan repayment packages, and relocation assistance to attract doctors. Some rural hospitals now advertise bonuses exceeding $250,000 for new hires.
Case Studies
- Rural Kentucky: A small hospital has been unable to recruit a full-time OB-GYN for over a year, forcing patients to travel 90 miles for prenatal care.
- Urban New York: Wait times for psychiatry appointments now exceed six months, worsening mental health outcomes in vulnerable populations.
- California: Large health systems are importing international medical graduates on temporary visas but face licensing delays.
Historical Parallels
The U.S. has faced physician shortages before—in the 1960s and again in the 1990s—but each time the system expanded training capacity and improved incentives. Today’s challenge is more severe, combining high demand, restricted supply, and structural burnout pressures in ways unseen in prior decades.
Long-Term Risks
- Health Inequity: Wealthier patients can pay for concierge care, while lower-income populations face shrinking access.
- Declining Trust: Long delays and poor access erode public confidence in the healthcare system.
- National Security: A weak medical workforce undermines readiness for public health crises, from pandemics to natural disasters.
Possible Solutions
Increase Residency Slots
Expanding federal funding for medical residencies could allow thousands more qualified graduates to enter practice each year.
International Talent Pipelines
Streamlining visa and licensing processes for international medical graduates could ease shortages.
Burnout Reduction
Reforming electronic record systems, reducing administrative burdens, and offering flexible schedules could help retain current physicians.
Incentivizing Rural Practice
Loan forgiveness, housing stipends, and career development programs can encourage more doctors to serve underserved areas.
Expert Commentary
- Physician Leaders: “We’re at a breaking point. Without structural changes, access to care will worsen dramatically.”
- Health Economists: “This is not just a workforce problem—it’s an economic problem. A shortage of doctors translates into higher costs and poorer outcomes.”
- Policy Advocates: “Congress must expand residency funding. The bottleneck is not medical school admissions but postgraduate training.”
FAQs
Q1: How severe is the U.S. doctor shortage?
It’s critical. Projections suggest a deficit of up to 124,000 physicians by 2034, with primary care and rural regions hit hardest.
Q2: Why can’t medical schools just admit more students?
They can, and many have. But without residency slots—required for licensure—graduates cannot practice. Residency capacity has barely grown in decades.
Q3: Can nurse practitioners and physician assistants solve the gap?
They help significantly, especially in primary care, but cannot fully replace doctors in specialized or surgical fields.
Q4: What role does burnout play?
A major one. Nearly half of all doctors report burnout, with many reducing hours or leaving clinical practice entirely.
Q5: What solutions are being proposed?
Expanding residencies, streamlining international licensing, incentivizing rural practice, and reducing administrative burdens are among the leading ideas.
Conclusion
The U.S. physician shortage is not a looming threat—it is already here. As hospitals scramble to recruit and patients wait longer for care, the cracks in the system are widening. Without decisive action—expanding residencies, supporting international graduates, reducing burnout—the healthcare system risks drifting into a prolonged access crisis.
This moment is pivotal. The choices made today by policymakers, educators, and healthcare leaders will determine whether the U.S. builds a resilient, equitable system—or whether millions of patients find themselves stranded without the doctors they need.